Stress and anxiety are a modern health crisis, and the problem is growing. Among the growing number of mental health conditions, Post-Traumatic Stress Disorder (PTSD) is a challenge facing today’s healthcare systems. New evidence has suggested a relationship between PTSD and sleep quality, and it appears that interventions focusing on sleep can assist in the management of PTSD. Sleep science, along with current medical research, has reached the point that practitioners are able to not only address the direct benefits of sleep, but improve outcomes of disease and other medical conditions. The relationship with PTSD and sleep is a complicated biological connection, and this article covers what you need to know regarding the importance of science and the practice of sleep monitoring.

The Vicious Cycle of Impaired Sleep and PTSD
PTSD is a mental condition where those who have experienced a traumatic event later struggle with daily functioning. Those affected are haunted by symptoms such as intense anxiety, graphic flashbacks, unwanted thoughts, and preoccupation of the traumatic event.
Those that have effective treatment can eventually live normal and symptom-free lives, but those that are severely affected may suffer for years with depression. The suicide rate of military-specific PTSD is especially alarming, and the National Institute of Mental Health estimates 7-8 Americans out of 100 will be affected by the condition at some point during their life.
The main obstacle with PTSD is that the condition is both affected by sleep quality and can impair sleep itself, creating a chicken and egg dilemma that practitioners struggle with. Often, those with PTSD have nightmares, rendering even the notion of getting a good night’s rest a dreadful idea. The current evidence is encouraging, but sleep disturbances from medications and substance abuse further exacerbate the condition of PTSD and must be factored into a treatment plan.
Efforts to improve sleep quality and duration to normative levels are instrumental on the road to recovery. Sleep, and even the pressure to sleep well, can backfire as an intervention unless a strategic approach is used, including patient education and sometimes pharmacology.
In addition to sleep hygiene, outside interventions such as exercise, psychological biofeedback, mindfulness training, and nature-based excursions can all improve sleep performance if implemented properly.
Inflammation, Biomarkers, and the Brain
While many events that are at the root of PTSD are kinds of physical trauma, many cases can be considered brain injuries with regards to inflammation. Although the research is unclear what precisely happens physically with a traumatic event, the end response beyond the emotional toll is often a change to the immune system and endocrine system.
Research on sleep disorders demonstrates an immune system impairment and physiological strain on the central nervous system. Impaired sleep and chronic inflammation are a primary mechanism to additional diseases such as chronic fatigue syndrome and other illnesses connected to sleep.
Several inflammatory biomarkers are associated with PTSD, and they often overlap the biological interaction seen with sleep disorders. Inflammatory markers C-reactive protein, TNF-Alpha, and Interleukin 6 (IIL-6) are commonly tested to infer a possible diagnosis or attempt to evaluate the severity of sleep disorders.
Research on PTSD and biomarkers revealed that sleep interventions are associated with affected patient symptoms. A comprehensive plan and continual effort in reducing systemic inflammation is paramount for living with PTSD, and for maintaining a healthy life.
PTSD responds to a combination of self-care, guided therapy, and sometimes medication. Each case is unique, but overall physical health is pivotal to successful treatment. Patient wellness, specifically exercise, nutrition, and sleep, determine much of the positive outcomes of PTSD.
Those patients who make a commitment to improve their sleep have the best chance in improving their symptoms over those that do not alter their sleep quality. Some patients, especially those with unique brain structures, may be predisposed to higher risks of PTSD, but today the research isn’t clear enough to determine those observations. In the meantime, focusing on brain fortitude from health seems to be the best hope in the fight of the condition.
Screening for PTSD and Sleep Disorders
Most healthcare professionals working with PTSD patients are managing cases from referrals rather than any type of screening process. Currently, no screening system exists that is considered best practice, and most cases are diagnosed from a combination of physical and physiological criteria, as well as criteria based on accepted research.
Sleep disorders are far more common and are similarly most often reported by patients to their primary care physicians or similar. Thus, the opportunity to tackle the problem of PTSD and begin treatment may require creative collaboration with the health and wellness market.
Sleep disturbances that are diagnosed by a professional and monitored by support staff can be a trigger to follow up with exploratory questioning. Short, repeated monitoring of sleep with baseline data, while not technically screening, can help identify those unaware of their condition.
It’s common that many victims of trauma are unaware of the diagnosis and condition of PTSD and are unable to ask for help, relegating their symptoms to a past event or being overly emotional. Awareness of PTSD is often too late, as many other chain reaction behaviors such as substance abuse and problems with relationships can mask the condition.
Continuous care and monitoring are essential for supporting trauma survivors. Relapse is a common and normal occurrence with PTSD, and additional monitoring after significant improvement is a treatment which caregivers can provide their patients. Due to the non-invasiveness of sleep monitoring, the opportunity to manage a patient for years is certainly possible, and likely necessary for severe cases of PTSD.
Unfortunately, many victims of traumatic events must see their PTSD diagnosis as a major part of their lives and must live with the condition for years. If management is combined with sleep, PTSD patients can reduce their symptoms dramatically and live normal and productive lives.
Managing and Treatment of Sleep and PTSD
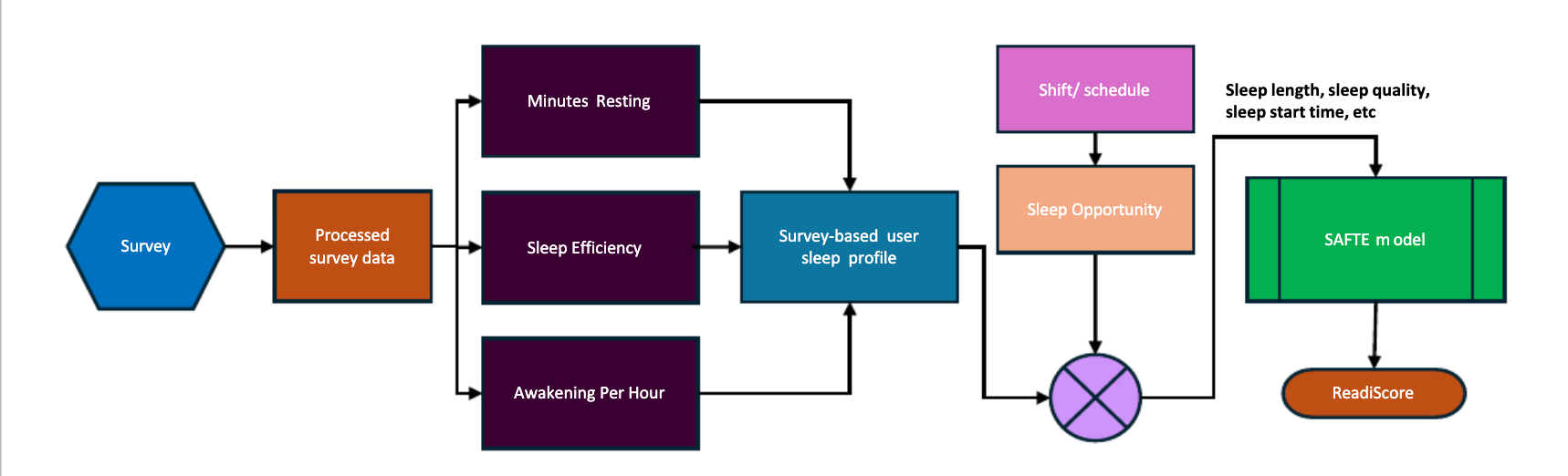
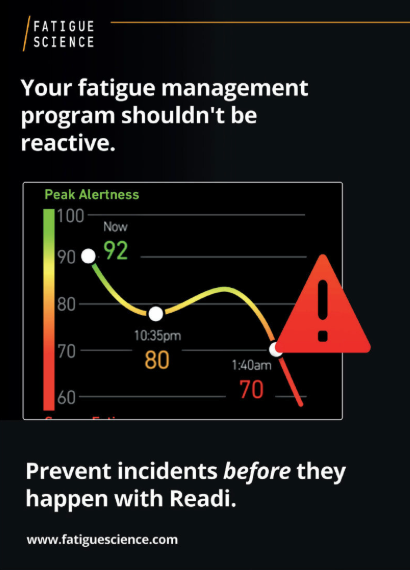
The complex interaction of variables and symptoms related to PTSD requires medical supervision, but the addition of simple sleep tracking can improve patient outcomes and help monitor progress. The current strategy supports the use of sleep management, and approaches that leverage the use of fatigue monitoring can show a direct cause and effect in some use cases.
Health care providers, specifically therapists working with PTSD patients, can combine conventional practices and more sophisticated sleep tracking when used properly. Therapists involved with the management of PTSD must use a comprehensive approach to reduce the severity of symptoms and to help with patient coping. PTSD is not a disease, it’s a mental health condition that is treatable if properly managed.
Sleep disorders often impair the recovery as well as exacerbate symptoms, so focusing on the direct trigger and the environment will improve patient quality of life. Sleep monitoring clearly has a role, but fatigue management extends throughout the day.
Focusing just on sleep alone is a very effective way to improve patient outcomes but extending monitoring beyond the confines of the bedroom is essential to maximizing patient results. Monitoring the entire daily rhythm of life can help improve the understanding of possible risk periods and patterns that increase symptoms.
New Hardware Options for the Fatigue Science Platform
Recently, Fatigue Science released the Readi™ app which introduced support for Fitbit and Garmin devices in addition to support for ReadiBand. This hardware agnostic approach allows the end user to choose a device that satisfies their personalized lifestyle. Data from Fitbit or Garmin devices now synchronizes with Fatigue Science’s proprietary fatigue algorithm, enabling medical professionals and health practitioners to monitor and support their PTSD patients.
Along with new hardware options, Fatigue Science’s Readi app and enterprise software platform empowers health care providers to manage large patient groups with research-grade precision. Using this platform, an individual or institution can monitor sleep, measure the impact of interventions over time, and perform detailed analysis with industry standard reporting.
Along with the Fatigue Science software platform, data can be securely synchronized with external platforms for even more insight. Going forward, Fatigue Science will continue to support the platform with new research and product development.
Capture a Baseline and Take Action
Sleep is a vital component to overall health and wellbeing with the general population. It can be argued that it is pivotal for those struggling with PTSD. Investing in a holistic and multi-faceted solution to the condition requires the addition of sleep monitoring, and Fatigue Science is committed to supporting patient care with a practical and powerful hardware option and web platform.
Practitioners that are serious about patient care and demand the most scientifically supported methods can reduce the severity of PTSD with sleep monitoring. Reducing systemic inflammation and improving sleep hygiene are direct factors in successfully treating PTSD.
Download our free eBook on the Science of Sleep for industrial workforces