Sleep apps: How reliable are they?
Are there any scientifically valid and reliable sleep apps? Prior to the new year, we referenced a study conducted out of Oxford University which concluded that mobile sleep tracking apps did not provide consistent or validated results. The Huffington Post also recently looked at some of the more popular consumer wearable gadgets that claim to monitor sleep and provided a similar conclusion.
Fatigue Science Founder, Pat Byrne, advises that people should ‘ask hard questions about the validity of all products we use’ and but even more importantly, challenges people to ask themselves exactly what they are trying to measure when looking to track and monitor sleep. He writes:
First, sleep is a complex process – When we sleep, how long we sleep, and how well we sleep directly affects our reaction time and ability to concentrate when we are awake. When you set out to measure sleep you have to ask yourself, What exactly am I trying to measure and how am I going to use this data? What am I trying to accomplish with the data?
As the Huffington Post points out the “gold standard” for measuring sleep is polysomnography (PSG). This is how sleep is defined and it is used to clinically diagnose sleep disorders. However, PSG is largely restricted to in-bed sleep clinics – meaning, to take advantage of this level of sleep measurement, a person must be referred and subjected to an overnight sleep study in a clinical, supervised, environment.
Actigraphy, on the other hand, can be used to measure individual sleep in any environment. The technology has been around for over 30 years, and is widely considered to be an acceptable alternate for sleep measurement. Actigraphy uses accelerometers (sensors that recognize motion) which can use wrist motion measurements to classify sleep and wakefulness. The technology is explained quite well by the American Academy of Sleep Medicine.
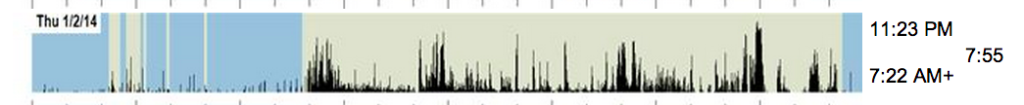
Actigraphy data from a Readiband
The key to obtaining reasonably accurate sleep results with actigraphy are the algorithms – built into the actigraph – which turn the wrist motion data into sleep data. The algorithm we use here at Fatigue Science with our Readiband is 93% accurate when compared to PSG in independent testing. Other actigraphy-based products use algorithms that have varying degrees of accuracy when compared to PSG.
If you are contemplating using actigraphy in any form, it is always helpful to ask the manufacturer for their PSG comparative studies – independent studies are even better. The Huffington Post article seems to indicate that the consumer fitness trackers are not very accurate. I have not read the research they are referring to, but if you are considering using a consumer device for sleep monitoring, I would recommend that you study the research.
Our business is helping organizations improve their worker safety and sports teams manage their athlete fatigue to improve overall performance in both the workplace and the stadium – having a highly accurate algorithm for our Readiband was central to being able to deliver our clients very objective and meaningful sleep data.
As the second part of a Fatigue Science analysis involves turning sleep data into a performance measurement (modelling reaction time and ability to concentrate) we need to ensure we are starting with highly accurate sleep data. Teams, players, and organizations value the information and insight they get by measuring performance in addition to sleep. Measuring performance takes into account the impact of circadian rhythms, jet lag, sleep duration, sleep timing, and sleep fragmentation to produce much more useful metrics. This performance measurement is something that none of the consumer fitness trackers or apps can provide.
Questioning the validity of any tool is good practice and your choice of actigraph should depend on what you are trying to achieve with the data, and how accurate you need the results to be.